You don’t hear much about mpox (formerly known as monkeypox) these days — and isn’t that great?
In the summer of 2022, there was a storm of warnings, declarations, articles, tweets, push notifications, and social media conversations about mpox. (After calls from various organizations to change the name to something less stigmatizing, the World Health Organization officially adopted “mpox” in November.)
At one point, the digital sphere was clogged with concern that this new global outbreak could have been a step toward the end of our days. And now, barely a peep.
Overall, there have been 29,646 mpox cases in the US as of Dec. 14, including 20 deaths, and more than 83,000 cases and 66 deaths worldwide (as of Dec. 20), many in countries that historically never had cases of the disease. Most of these cases were identified in gay and bisexual men, with the greatest danger of severe illness posed to those living with certain autoimmune conditions, including HIV. Particularly in the US, Black and Latine men have been disproportionately affected by the current mpox outbreak.
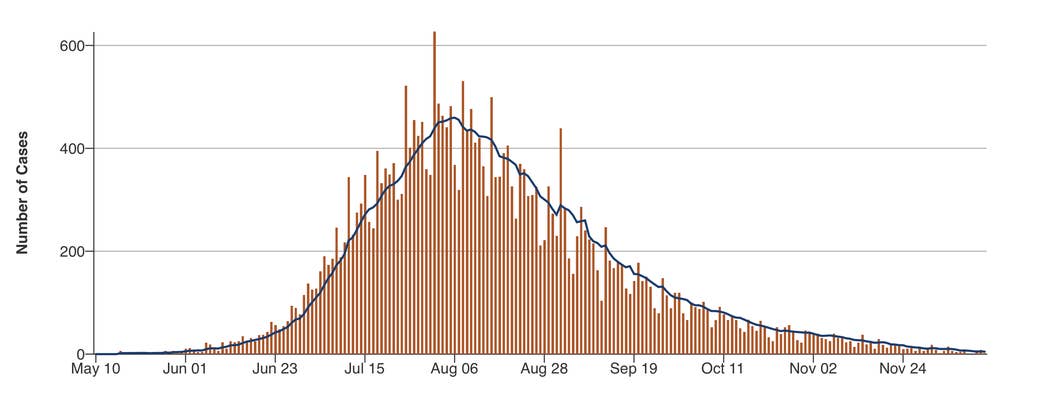
Cases are way down and trending in the right direction. The highest single-day case count in the US for mpox was 635 on Aug. 1, and the highest seven-day average was 462 on Aug. 6. Compare those figures to the latest data from the CDC, where there were less than 10 cases most days in early December. Can’t argue with data; the tides seem to have turned.
In fact, based upon this success, US Department of Health and Human Services Secretary Xavier Becerra announced on Dec. 2 that the agency would not be seeking to renew its public health declaration for mpox.
“From the outset of the mpox outbreak, the Administration pulled every lever to stop the spread of this virus,” he said. “Given the low number of cases today, HHS does not expect that it needs to renew the emergency declaration when it ends on January 31, 2023.”
This is all great news, a cause for celebration! But it’s also worthwhile to reflect on what worked — to take a closer look at the public health and grassroots efforts that turned mpox from a frightening and fast-spreading outbreak to the pandemic that wasn’t, all in the course of six months.
This success was the result of a coordinated, agile, science-informed effort: government officials who listened and responded to the community, private organizations that stepped up to educate and connect, and individuals — almost entirely in the gay community — who heard about the risks, got vaccinated, and changed their behaviors. In addition, efforts were made to mobilize and stretch the supply of an existing vaccine as well as approve a drug called tecovirimat (or Tpoxx), known to be effective against the virus.
A quick recap on how mpox cases exploded around the world
In 2022, there was a global outbreak of a large number of mpox cases in countries where the virus had, in the past, only caused isolated outbreaks or a handful of cases, usually in travelers. (The virus was first identified in 1970 and has generally caused smaller outbreaks — dozens or hundreds of people rather than tens of thousands — in 10 countries in Africa. The virus is found in rodents in some countries and can jump to humans to cause outbreaks.)
The first reported cases in the current global outbreak were in the United Kingdom on May 7. Then, further clusters appeared across Europe, mostly among gay men or other men who have sex with men. The outbreak spread further across the Atlantic; the United States eventually became the country with the most documented cases in the world.
In response, targeted educational and vaccine campaigns were instituted, and a couple months later, the World Health Organization and White House declared mpox to be a public health emergency, which helped drive the funding, attention, and coordinated response necessary to combat the virus’s spread.
People who get mpox experience symptoms with a range of intensity, some with relatively mild and isolated lesions and others with unbearable pain. The most common mpox symptoms are fever, chills, swollen lymph nodes, and fatigue, followed by skin lesions that can get progressively more painful before they heal.
People who are pregnant, under age 1, or who have a weakened immune system or a skin condition, like eczema or atopic dermatitis, are at risk for potentially severe mpox infections.
On Aug. 2, at the fever pitch of concern about the outbreak, the White House created a National Monkeypox Response office, naming Robert J. Fenton of FEMA and Dr. Demetre Daskalakis of the CDC as coordinator and deputy coordinator.
Fenton’s work at FEMA was crucial to the success of the US COVID-19 vaccination program. Daskalakis has made legendary contributions from community care to public health in the fight against HIV/AIDS.
When appointed by President Joseph Biden, Fenton and Daskalakis were given a goal to completely eradicate mpox in the United States. The task seemed daunting if not futile at the time, with many infectious disease experts saying that the US had already passed a point of no return for preventing this virus from becoming endemic, or one that would continue to circulate and cause outbreaks despite our best efforts.
Three months into their appointment, the coordinator and deputy coordinator seem calm, assured, proud even — and rightfully so.
“I would say that we have turned the corner, and the numbers continue to work in a declining fashion,” Fenton said.
“We are in such a different place than the last time I talked to you,” Daskalakis told BuzzFeed News. “You know, it’s kind of exciting to have this conversation. Our goal set by the president is still our goal, and we’re now down over 93% from the peak of the outbreak. Now, we’re pushing toward a point where monkeypox isn’t a part of everyday life in the US.”
Mpox didn’t just disappear

Controlling the mpox outbreak has been all about community coordination and having leaders who empower experts to make science-based decisions. In addition, a collective of individuals and organizations banded together to ensure that information was widely disseminated about symptoms, risks, and vaccine availability.
Nowadays, pretty much anyone can walk up and get a mpox vaccine. Many sites offer walk-in shots with no questions asked, while some may require you to self-attest to your risk of infection. This is a huge shift from just a few months ago, when lines in many cities stretched for hours through parks and around city blocks. Supplies were low, and it wasn’t uncommon to be turned away even after waiting in line. Some complained the systems were racist and classist.
When the White House response team was put into place, they started listening and working to address the issues. They were able to do this because they were empowered with the ability to change course without a lot of red tape.
“It takes science, humanity, leadership, and political will to focus on these events,” Fenton said. “It takes a tremendous amount of education. You need to be able to leverage and utilize science.”
Such adjustments began with a switch to intradermal injections, which addressed vaccine shortage by allowing the existing supply to stretch up to five times further. At the beginning of August, there were no intradermal doses being given; three weeks later, intradermal injections accounted for 74% of the vaccine being administered nationally, even though administering the vaccine in this way, which uses a very fine needle to introduce the vaccine just under the skin, requires specialized training.
Immediately after the announcement to switch, there was some concern about whether the science behind the decision was strong enough. One article in the Atlantic went viral saying the entire US mpox vaccine strategy hinged on just one study. Then, after intradermal injections began, some complained about the mark they were leaving behind on their forearms (this technique can create a small bubble in the skin that could leave a scar). All the while, Daskalakis said, the White House was listening.
“Community said, we need to better understand what the thought process was behind moving to intradermal. So, we put out an FDA document that actually goes over that step by step,” he said. “Community said, we don't want the mark to be on our forearm. What about moving the vaccine site? So, we figured out alternate sites with the FDA and CDC.”
Daskalakis, whose work has historically been focused on HIV, seems to have a particular appreciation for how this White House responded.
“Coming from the HIV experience and doing work with the population, and all the challenges we have faced. And then, having the leader of the free world tell you, please focus on gay and bisexual men, and make sure that you focus on Black and brown people to end this. This is an infectious disease doctor’s dream come true,” Daskalakis said.
Most mpox vaccination efforts in the US have been run by local and state health departments. In some cities, like DC, vaccination appointments were once only available through online portals, which would sometimes crash when word got out that a new batch of slots had opened. Citizens complained that this system was favoring white people and higher earners.
Dr. Kimberly A. Sommers, interim chief science officer for the DC Health Department, explained one way the agency responded.
“People let us know, and we listened,” she said. “Instead of requiring everyone to go through the website and enter a bunch of private information, we started offering more walk-up clinics. And once we did that, we found a noticeable increase in vaccine uptake in our communities of color.”
Beyond vaccination, the significant drop in cases can also be attributed to gay and bisexual men heeding a call to limit their sexual partners, as well as immunity of the previously infected.
After it was widely broadcast that mpox was spreading primarily through sexual contact, experts asked people at risk for contracting the disease to modify their behaviors, essentially to avoid casual sex. On Aug. 22, the CDC published a report of a survey of gay men, 50% of whom reported reducing the number of sex partners and one-time encounters in the first half of the month. Furthermore, evidence suggests that previous infections with mpox are believed to confer immunity to future infections. That means, once you get it, you won’t likely get it again.
Incidentally, one of the biggest connectors for information sharing in the US and around the world is also an app that many gay men use to hook up: Grindr. One department at the company, Grindr for Equality, has a stated mission to make connections with community organizations with the goal to keep the app’s users around the world safe. This includes making inroads in locations that are politically unfriendly to LGTBQ+ people. It also includes addressing any type of outbreak or health issue affecting the community, including HIV, meningitis, and COVID-19.
“There were a lot of people who received their first really good information about COVID from Grindr for Equality, especially if they were living in a country where the government was denying it,” said Jack Harrison-Quintana, who directs the program. “Then, when mpox kicked off, we already had our playbook.”
He refers to Grindr as the “connective tissue” in a certain channel of the mpox information campaign. Since May, Harrison-Quintana and his team have been working with the European CDC, the American CDC, and other health agencies around the world to get word out about mpox. Local agencies craft messaging alongside representatives from the app that are then sent out to all users in a particular location.
As one of the earliest adopters globally of information sharing during this year’s mpox outbreak, Grindr was faced with a significant challenge. In many cases, the company just didn’t have the answers to what its users wanted to know.
“We started our messaging in mid-May,” Harrison-Quintana said. “It wasn’t until several months later that President Biden finally declared a public health emergency. I was in this position where I was messaging all of these people about this problem, and I just didn’t have any solutions.”
The effort to end the mpox outbreak is still ongoing

In his Dec. 2 statement that the HHS would not be renewing the mpox public health declaration, Secretary Becerra stated that the agency would still be continuing its efforts offering services to control the outbreak as needed.
“We won’t take our foot off the gas,” he said. “We will continue to monitor the case trends closely and encourage all at-risk individuals to get a free vaccine.”
In the remainder of time that the declaration remains in effect, the agency is working with local jurisdictions to ensure that the expiration will not hinder ongoing efforts to combat the outbreak.
Though case numbers nationwide in the US are now extremely low, experts have observed small clusters concentrated in specific regions, including parts of Texas and Southern California. Accordingly, the White House and CDC are focusing their efforts, zooming in for localized vaccination and education campaigns.
“We are hyperfocused on those local areas, ensuring that there's better vaccine uptake to ensure that we are prioritizing diversity and equity in our outreach,” Fenton said.
“There are over 3,000 counties in the United States, but only 81 had any monkeypox cases in the past two weeks,” Dr. Jonathan Mermin said. He is the CDC’s director for the National Center for HIV, but this year, he’s been focusing on mpox.
Although there were serious concerns about mpox spreading in children at the end of the summer of 2022 when kids went back to school, that didn’t materialize. Overall, there have been 83 cases in people under age 18, or about 0.3% of all cases, according to a CDC report released in November.
These cases are mostly from skin-to-skin contact with caregivers; the virus is more difficult to spread than, say, COVID although mask-wearing can also help prevent the spread of mpox.
Mermin is hopeful and optimistic for the future of the outbreak, but he also acknowledged that in our global society, the goal to end new mpox cases in the US will be dependent on the work done to control the virus overseas.
“Even if we move toward eradication, it is still possible we will continue to see new infections in the United States, whether coming in from other countries or places where a positive case went untested,” he said. “We need to fortify the public health system to be able to respond rapidly to those events, so they don't spread further.”
The global conversation is also ongoing at Grindr, where Harrison-Quintana is preparing to send a message about vaccine availability in Chile. He is also currently working with the Pan American Health Organization to craft a message about mpox that will soon be broadcast to all Spanish-speaking users, even in places where no vaccine is available.
“This will go out to a lot of places where many people are still like, what is monkeypox?” Harrison-Quintana said. “That’s really where our focus needs to be right now.” ●
